- To explain to people, as fully as possible, where I'm at and where I've been, personally.
- To raise awareness of my core discoveries (much of this may apply to many people).
- Possibly help others take short-cuts (I've already spoken to a few with similar issues).
- To review what I've looked at so far, reminding myself and reappraising with a critical eye.
The grey sections contain stand alone information, e.g.:
As usual, I became a little mired in detail. Perhaps I was guided by a previous whim to make an all-encompassing 'cheat sheet' type resource for 'histamine intolerance' (a complex issues with even greater uncertainties than other similar problems). It is almost entirely unrecognised by GPs in the UK.- Food intolerance may affect 45% of the population, causing a surprisingly wide variety of easily fixable, idiopathic symptoms, throughout the body (headaches, rashes, itching, diarrhoea, and vomiting...).
- Histamine intolerance may affect as many as 1 in 10 (1 in 100 at lowest estimate). Almost always co-morbid with another food intolerance/disease [source].
+ A Poor Boy, So Sorry for Himself:
Back in 2007, with Cybernetics degree slipping my grasp, due to deteriorating mental energy and my milieu of inter-related problems (see my 'Illness CV'), I said to myself:
- 5 years from now I will definitely have found something to give me significant relief from my problems. I had something like an Orexin nasal spray in mind, to aid waking and wakefulness (but despite amazing results in monkeys, the safety trials don't seem to have been happening, since both compound and delivery mechanism are non-patentable).
- By the 10 year mark I was betting I'd be effectively cured! I am a disciple of the gods of accelerating change, after all.
 |
| Out of juice crossing the room (Jan 2008), or that other frequent trap - having to bend down for something. There happened to be a camera to hand in this instance. |
IBS-D, to be precise.
+ Food Intolerances and Testing
I had already been chatting with an interesting guy in Los Angeles (one of my alliance co-leaders in Lord of Ultima) about the naturopathic (i.e. non medical) treatments he claimed are helping his ADHD, currently treating for chronic yeast infection with traditional remedies including ACV (apple cider vinegar). I was naturally sceptical of his reasoning (with no conventional evidence in support), but the wheat and dairy exclusions were familiar, so after only 2 days of urgent WC visits I made the necessary changes and the GI problems stopped!
I previously attempted going dairy free back around the time I launched this blog (and it's two companions - short lived): "This week I shall mostly be avoiding dairy!" (2006-12-05). But I barely gave it any time before: "So the cow milk related product embargo lead nowhere and I blatantly couldn't be arsed avoiding wheat! I have sent off for a £20 finger prick type testing kit,.."
Although I did try wheat free the following year (2007-05-13), but again:
"Well i started a follow up of wheat free (just in case my negative blood test for Coeliac the other month wasn't up to scratch) which lasted til after breakfast when i nearly fell asleep (and i'd only had bacon, scrambled egg, mushroom and baked beans!)."
My mistake is now obvious: I didn't give it nearly long enough to kick in! Also, the food reactions, which I've carefully observed this time, are not specific to what I have just eaten: eating seems to move digestion along causing the 'bad' food from 16-24 hours ago to reach the point where it actually causes trouble (presumably the large intestine). Delayed reaction.
This time around the threat of IBS was sufficient to continue exclusions for a couple of weeks. Soon after this point I was scrabbling around the loft (a long crawl space under the sloped roof, waist high at it's tallest, stuffed with heavy boxes), looking through everything (twice) to find old school reports ready for my upcoming ADHD assessment (2013-04-05)... and I realised how much better I was!: previous attempts at such confined exertions quickly transitioned into laying down, on the job, for a couple dozen minutes until I could summon the strength for a gruelling tactical retreat. What's more, I actually found what I was looking for, eventually, inefficiently, but triumphantly!
The most consistent symptoms improvements I'd ever experienced compelled me to set aside medical dogma and some scepticism. These sensibilities had halted me taking things any further with my "positive" reaction with the £20 blood drop intolerance indicator from half a decade ago (I felt a cynical and a little cheated, realising that practically all tests would show up something). So I finally took a £300 punt on a Yorktest, full food intolerance, IBS test panel with telephone follow-up.
 |
| IgE vs IgG - P.81, Optimum Nutrition For The Mind, Patrick Holford |
The lab work itself is solid and respectable, but it's meaning and interpretation are problematic. A positive result only really indicates contact between your immune system and food substance in question (or sufficiently similar proteins/markers).
 |
| Blood sample, absorbed into stick and thumb pressed lance. |
However, this study was criticised directly. Also, The House of Lords Science and Technology Committee report of 2007 stated in section 8.35 that there was "...limited evidence to support [York Test's] claim." and "We urge general practitioners, pharmacists and charities not to endorse the use of these products until conclusive proof of their efficacy has been established." Allergy UK seems to no longer endorse/promote York Test, so this testing is still a grey area.
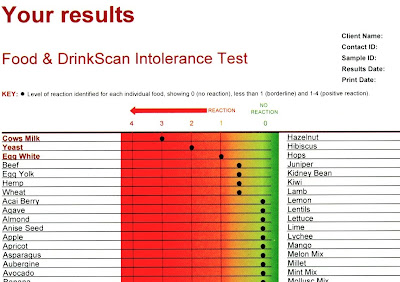 |
| My notable York Test IgG reactions from my full report. |
Yeast Intolerance Exclusions (awkward!):
- Baker's yeast: all breads (except wraps, soda bread, crispbread, some pitta).
- Brewer's yeast: beer, wine, cider (distilled, clear, spirits ok: vodka, gin).
- Vinegar (i.e. acetic acid): all pickles, mayonnaise, chutneys, salad dressings.
- Fermented foods: soy sauce, sauerkraut, miso, sour cream, yoghurt, buttermilk, kombucha.
- Stock, gravies, extracts (e.g. Marmite).
- Surface yeast on: some fruit (e.g. grapes), dried fruit, old food (left-over).
- Misc: tofu, quorn, hydrolysed protein, MSG, some citric acid, (B Vitamins).
[From allergyUK, confirmed by York Test.]
The telephone nutritionist seemed pretty well prepared for my specific results, reeling out a sting of websites, books and a dismaying tirade of unexpected yeast related food substances. This will probably be because dairy, wheat/gluten and yeast are the top 3 most common, it seems. With alcohol the 4th in Allergy UK's list: for 6 months leading up to my new IBS I'd had problems with even modest drink intake (up the whole night feeling, being, quite ill).
So, even without doing any actual testing you could probably get at least 60% of people's intolerance symptoms improved by just having them avoid a couple of the top trouble makers.
 |
| Varying acidity of the GI tract (from here). |
The dietitian, to whom my GP referred me (with few expectations) could manage no more than whipping out a FODMAP leaflet too, pointing at the little diagram where the bad foods march right on down the track to the problem zone. We know from the Lords report that finding an NHS "...dietician who understands food intolerance is extremely difficult on the NHS".
I am now due to visit an allergy specialist next month (5 months down the line from first GP contact about this issue), again with little expectation. Pretty disappointing, if ",..up to 45% of us are affected by food intolerance,..", from a Guardian piece (2011), which also quotes the Lords Equiry saying: "...Britain was "the laughing stock of Europe", and many patients go untreated".
+ Histamine Intolerance:
This may sound exotic to most English speakers, but is well recognised in continental Europe (Germany, Spain, Switzerland, etc), where the majority of the population has supposedly heard of it. Awareness seems to be spreading to our shores via the Netherlands (mostly fluent English speakers who also write scientific papers in English as standard), and via UK natives with a foreign contacts (some of the authors listed below).
This one came at me via another lucky break, when a Dutch friend specifically messaged me about her friend who had discovered histamine intolerance (i.e. HIT) as a cause of long standing headaches/migraines. These are a very common symptom of this dietary intolerance, the others include dermatitis (eczema, urticaria) and obviously, gut problems (but not necessarily).
Histamine's Normal Bodily Functions:
It's an overlooked neurotransmitter - most closely tied to alertness/wakefulness. Histaminergic neurons, from the hypothalamus, start to fire right before waking up. Suppressing their action, with old style anti-histamines, causes sedation. Mirtazapine caused me a massive hyper-somnolence side-effect via this route.
Stimulates stomach acid, GI tract motility and can mediate evacuation (both directions) of perceived poisons (e.g. scomboid food poisoning from spoiled fish).
Triggers local inflamation, increasing membrane permeability (e.g of capillaries) to allow WBCs, etc to mount an immune response. Released from immune system mast cells (in tissue) and basophils (WBCs) when triggered, via IgE receptors, to 'de-granulate'. Essential for wound healing.
Broken down by 2 enzymes:
- DAO (diamine oxidase) - in small intestine and blood.
- HNMT (histamine-N-methyltransferase) - inside cells/tissues, CNS. Uses SAM-e.
Opposes adrenaline, causing vasodilation and bronchial constriction. And vice versa: EpiPens are used to treat anaphylactic shock.
It's an overlooked neurotransmitter - most closely tied to alertness/wakefulness. Histaminergic neurons, from the hypothalamus, start to fire right before waking up. Suppressing their action, with old style anti-histamines, causes sedation. Mirtazapine caused me a massive hyper-somnolence side-effect via this route.
Stimulates stomach acid, GI tract motility and can mediate evacuation (both directions) of perceived poisons (e.g. scomboid food poisoning from spoiled fish).
Triggers local inflamation, increasing membrane permeability (e.g of capillaries) to allow WBCs, etc to mount an immune response. Released from immune system mast cells (in tissue) and basophils (WBCs) when triggered, via IgE receptors, to 'de-granulate'. Essential for wound healing.
Broken down by 2 enzymes:
- DAO (diamine oxidase) - in small intestine and blood.
- HNMT (histamine-N-methyltransferase) - inside cells/tissues, CNS. Uses SAM-e.
Opposes adrenaline, causing vasodilation and bronchial constriction. And vice versa: EpiPens are used to treat anaphylactic shock.
Alcohol is a top trigger here, with multiple mechanisms of action, which struck a chord with me. Plus, I was already excluding half the items on the list. So when I seemed to have an IBS reaction to eating a large volume of hot chilli flavoured foods, and then another in apparent relation to a tuna steak dinner (a little later), I decided this previously obscure condition held far too much explanatory power to ignore.
Actually, "Histamine" is the 5th item on the "common food intolerances" list, but HIT is poorly understood, with few books or authoritative resources available, and no Wikipedia article (as of writing). It's subtle in it's details, with much variation in personal tolerance, hence great variation and inaccuracy of food/drink exclusion lists online. There are no definitive tests for this either; the only proven approach is careful use of a food diary as foods are re-introduced after a strict exclusion period (of several weeks).
Such a process might also help identify intolerance to salicylates (which is fairly common) plus benzoates, tartrazine, possibly oxalate, nitrates, tyramine (although I don't know anything about these last ones). A more targeted elimination diet might look for fructose mal-absorbsion (non hereditary) or lactose intolerance (completely distinct from troubles with casein proteins in dairy). Digestive tests for these last two, but they are supposedly ambiguous, given that everyone has different enzymatic capacities, which fall off with age too.
HIT seems to be female dominated: sufferers and authors. These three ladies are the most prominent sources of English language information on the subject (that I've found), on web and in Amazon's book store:
.png) |
| Genny (source). |
She's a freelance TV producer, who's worked for the BBC, and may have helped massively in drawing attention to this diagnosis via an article on her in the Daily Mail (2011). This May (2013) her co-authored "Food Intolerances: Fructose Malabsorption, Lactose and Histamine Intolerance" was released too.
 |
| www.histamine-intolerance.info/ |
But, despite one third of her 200 page book being reproductions of abstracts from related scientific papers, she fails to support her thinking with anything more substantial than personal anecdote. So while she's collected a lot of information and it raises some interesting questions, it's presented poorly and has no recognised authority beyond internet research. So I do not recommend this book!
Low Histamine Chef (Yasmina Ykelenstam) has put an inordinate amount of effort and materials out there for sufferers of histamine problems (even replying to my annoying comments in her Facebook group). She's an (ex) BBC journalist who recently figured out she has
Her recent telephone interviews with Dr Janice Joneja are most authoritative and clear sources of information on HIT and food exclusions: Part1, Part2 (both with transcripts; highly recommend). From her years of work work on allergy (and with clients) I think Dr Joneja must be responsible for the common use of the 'bucket' (or barrel) analogy with HIT.
Unlike in IgE allergy or lactose/fructose intolerance, etc, reactions to histamine depend upon one's sum total histamine intake/burden at that point (i.e. the level in your 'bucket'/body). So while a questionable fish course may have so much histamine that it will always trigger a reaction, a couple of tomatoes, or a small glass of spirits, may or may not tip things over the edge. Hay fever season, psychological stress or even sunshine may add enough background histamine to make the difference. This adds to the complexity of reconciling dietary exclusions, but can also give sufferers far more leeway (to go slightly off-diet) once the major contributors to their raised histamine levels are under control.
 |
| [Click image for full size!] Total bodily histamine is analogous to the water level in a bucket (full is bad!). Diagram by me. Information primarily from the Dr Joneja interviews (grey writing is uncertain). The order of symptoms (or even their presence) is very dependant on the individual. This presumably relates to inherent susceptibilities/variations in the function of each organ system. Aerobic exercise also releases histamine, and intense exercise can trigger anaphylactic shock in certain circumstances . |
If your problem stems primarily from lowered DAO secretion (or activity; i.e. SNPs encoding the enzyme's structure), then histamine 'liberator' foods might not be such a problem (aside from any intrinsic histamine content). Incidentally, direct serum DAO level testing is said to be pretty meaningless.
Just as digestive enzymes can be taken (with food) to help compensate for a lack of lactase, etc, there are products that claim to to do similar with for histamine: 'DAOsin' (or DIAsin in the Europe), branded as 'Histame' for northern America, contains "0.3mg [DAO] as porcine kidney protein concentrate" per pill. I bought a bottle of 30 capsules from Amazon for £33 (yes, over £1 a pop!), but it's no longer available. Perhaps legal issues caught up to UK resale.
At any rate, this supplement does not seem to be a magic bullet (quite aside from it's expense). It may have shown efficacy, but the studies are Austrian and in German. I think it might have helped me avoid gut reactions, but I've had incidences of the usual fatigue and cognitive problems the following day, regardless. Genny's book also states "the tablets only work sporadically" for some, and she (like me) has only used them as a last line of defence (when forced to eat out, etc).
A single large dollop of DAO is presumably not going to mix as well with incoming food as the continual supply produced by a healthy intestinal mucosa (the gut lining, which also secrets blood-borne DAO). Additionally, since histamine regulates intestinal movement(s), there's a lot of scope for upsetting balance (which I've observed), and unknown long-term possibilities.
DAO may be dependant on B6, with "riboflavin [B2], zinc and magnesium" as co-factors, according to Genny's "What HIT me?" (since Wikipedia is a dead loss here). While Vitamin C helps too, deactivating histamine (and also preventing UV-B stimulated histamine release, in direct sunlight).
Anti-histamines are only recommended to manage symptom crisis, since they merely block the effects of high histamine for a while (by clinging to receptors H1, H2, for example). In fact, hiding high histamine away is counter-productive, since it seems to stop the body breaking it down and/or stimulates further (compensatory) release.
Other notable HIT resources:
- "Histamine and histamine intolerance" (2007 - Laura Maintz and Natalija Novak).
- Dr Janice Joneja's allergy fact sheets, particularly the Histamine Intolerance pdf.
- A massive academic paper summarising everything about histamine in the nervous system.
- HealthyPixels - A general health blog with a great article on HIT, drawing on many sources.
- Hitting on HIT - A decent blog about HIT. They made some meta-lists for food exclusions based on a summary of several Google results, but the scoring here may just make the result even less reliable, since there is much anonymous copying between sources (where memetics may bias things) and it doesn't account for the complete absence of foods, from lists (as opposed to explicit inclusion).
- Dutch list of high histamine foods - showing values. See page bottom - note the orders of magnitude differences in histamine levels; certain cheeses, meats and red wine (that are fine for everyone else) are like a nuclear histamine bomb, compared to veg that is slightly problematic.
- Bitelog - (or similar) to search up the 'histidine' (and other nutrients) content of various foods. Again you can see clearly how much more potential high protein foods have for (rapid) dangerous spoilage. (Note: everyone needs good quality protein!; just be extra careful with it.)
The Histamine Link:
I have been thinking that I fall into the category of digestive (DAO) insufficiency. Assuming my mast cells (and HNMT activity) is fine, since I do not have any noticeable allergy-style reactions: skin rashes, eczema, urticaria, pruritus (itching), acne rosacea, wheals, asthma, runny eyes, flushing and severe sweating, and the scary sounding symptoms Yasmina's experienced. However, I could be misinterpreting this.
HIT also seems to cause generally low blood pressure; histamine causes vasodilation (via H2 activated smooth muscle relaxation). Tension type (non-aura) migraine may then results from maintaining cerebral blood flow and arrhythmia/racing-heart too, as a result of compensatory use of adrenaline. My low BP has been commented on a couple times, and orthostatic hypotension (dizziness with greyed vision when standing) has been a common occurrence when I'm weakest, exacerbated by several medications.
Compulsive/excessive sleep and extreme tiredness after meals is something Genny masterman gives anedotes about (unavoidable napping on a row boat while filming on location). Persistent fatigue, unexplained weakness (and low body temperature) are amongst Yasmina's long list too. "Cognitive impairment/brain fog" is a big one, that she's complained about elsewhere too, and the most damning of my symptoms, right at the top of my 'Illness CV's. She's also had mania and repeated problems with insomnia, that seem to plague other allergy sufferers.
I first read about possible issues with histamine in Patrick Holford's "Optimum Nutrition for the Mind" where he talks about the work of Karl Pfeiffer (1908–1988). Pfeiffer worked a lot on schizophrenia, sub dividing suffers based on histamine status: 'histadelia' (elevated serum histamine and basophils) or 'histopenia' (opposite extreme) and/or 'pyloria' (excess B6 & zinc excretion). Treatment focused on high dose supplements.
His work was not adopted by mainstream medicine, and Holford is certainly a controversial figure (who's under-qualified considering his income from selling supplements and health advice).
Note: 'histadelia' symptoms list is from Diagnose-me.com, an online expert system that I tried out in 2007. I answered the 1000 odd questions, but didn't think much of it's suggestions (at the time) of: detoxification requirement, Dysbiosis, IBS, etc.
Histmine, like many organic chemicals, plays an entirely separate (and essential) role as a neurotransmitter: a relatively tiny number of histiminergic neurons 'project' axons throughout the brain, stimulating release of dopamine, nor-adrenaline, etc for wakefulness. They're tangled in with wakefulness sustaining orexin neurons (lacking in narcolepsy). Hence why anti-histamines are well known to cause extreme drowsiness, sometimes used specifically as sleep aids. Second generation anti-histamines were purposefully designed not to cross the blood-brain barrier (BBB). This protective coating of cells is essential in stopping your thinking medium being washed out by the deafening background noise of bodily processes, so it's hardly surprising that "Histamine hardly passes the blood-brain barrier (751),..".His work was not adopted by mainstream medicine, and Holford is certainly a controversial figure (who's under-qualified considering his income from selling supplements and health advice).
Note: 'histadelia' symptoms list is from Diagnose-me.com, an online expert system that I tried out in 2007. I answered the 1000 odd questions, but didn't think much of it's suggestions (at the time) of: detoxification requirement, Dysbiosis, IBS, etc.
So it was odd that high bodily histamine levels seemed to be causing neurological issues that sounded like elevated brain histamine; like 'histadelia' (see greyed note)....
But then if blood levels are very high, some might be leaking through. And more pointedly, the BBB can be 'opened' by mast cell degranulation, increasing it's permeability, allowing white blood cells in to help clear up severe infection. This extreme response causes side effects though (e.g. meningitis), so usually microglia/astrocytes in the BBB keep things in order, and keep us thinking clearly. A regulatory failure here might be a cause of 'brain fog'?...
However, it is acknowledged that schizophrenics demonstrate elevated brain histamine, and anti-histamines, in large doses, may help treat them.
But, if anything, it seems like my brain histamine is low, with long sleeping and difficulty waking, and excessive daytime tiredness/weakness. I had hypothesised (i.e. pulled supposition out of the air) that my BBB is doing it's job fine but high blood-histamine (from low DAO) was leading to whole body HNMT up-regulation (if such is possible), to help handle the histamine. Hence lowering brain histamine - HNMT is the main de-activating enzyme in the CNS (and liver, I think)...
...But there are other, more direct, explanations, that I hope to explore in Part 2, along with the beckoning promise of a bottom up revolution in medical care.



No comments:
Post a Comment
I'm very happy to see comments, but I need to filter out spam. :-)