This post follows on from my Part 5 Covid blog, which enumerated the problems with, and causes of, UK's apparently reckless re-opening. In the last section (I), I'd been examining the apparent downturn in cases, around the time of our "freedom day". It now looks clear that we were really seeing the end of the football peak (with a big pinch of school-kid case isolation, then finishing for summer) - a bonus peak on top of an overall continuing (slow) upwards trend in cases. Which has plateaued for now, probably (until football gatherings and school start up again, within the month!):
 |
| [Fig.1 - GovUK] Official stats show cases steady at ~25k/day, hospital admissions ~700/day. |
The official R number, for rate of Covid spread, today is 0.8 to 1.1. I think this is averaged over a time period including some of the brief case drop. So, it looks like R = 1 would be a better approximation of our momentary trajectory. Which is pretty bad, given the high incidence of disease. But fairly ideal for us to take a look and see how far we are from herd immunity (section J, directly below). We're definitely a good way off, because we're at an effective R of ~1, while the population is still being relatively cautious, still a lot of mask use, summer holidays and no football, etc. So we should be able to work out how much of a reduction is coming from these NPIs (non-pharmacological interventions, i.e. stuff other than vaccines).
Actual calculations and results in point (6).
Update 2021-08-14: Summary of the APPG conference call that triggered "herd immunity mythical" headlines, catching the general public up roughly, to what I've concluded here. See (B) below.
Update 2021-08-19: new and clarified information on vaccine effectiveness, section (C).
◄A► Calculating Population Immunity (is Hard!):
The exact degree of overall immunity is pivotal for calculating the effective R value. So as to accurately modelling and forecasting the rate virus spread (and help decide on the degree of mitigations needed). But there's been a lot of big unknowns for immunity to Delta: (1) how effective is each vaccine; (2) how much of a reduction in transmission is there for infected cases who have also previously been vaccinated; (3) how many people have been previously infected in each age group; (4) how protective is past infection; (5) how much does immunity wane over time, in each case? (6) Working the numbers for an estimate.
Here we're assuming all infections to be contagious cases, and equating the two (as there's not solid data for transmission, specifically). Which might be a significant departure from the reality. E.g. mild cases could be far less contagious, after vaccination, or asymptomatic cases may be going undetected more often, while still being very contagious, etc.
(1) Vaccine effectiveness vs Delta - Studies vary significantly, between countries. Probably mostly due to statistical idiosyncrasies of the data sampling, timing and location of outbreaks, etc. But also affected by time since vaccination and the schedule of injections used: UK at 8-12 week delay might have ended up more effective than the recommended 3 weeks, e.g. used in Israel. But in all instances we're seeing a drop in effectiveness against infection with Delta, vs Alpha or original strain. But still very good protection verses hospitalisation (and death).
Verses infection (from video linked below):
• Pfizer BioNTech, 2 doses: 64% - 88% (~80% average). 1 dose: 33% - 56% (~45% average).
• AstraZeneca (Oxford) 2 doses: 60%. 1 dose: 33% - 67% (50% average).
 |
| [Fig.2.a - MedCram YouTube] Pfizer effectiveness data (from UK, Canada and Israel) all depicted in this graphic on page 19 of the CDC's leaked presentation [Washington Post via Hannah Davis, Twitter]. |
 |
| [Fig.2.b - Gov.UK via Twitter] VEEP (Vaccine Effectiveness Expert Panel) consensus narrative 16 July, updated 4 Aug, gives (somewhat inexplicably) more optimistic figures verses symptomatic infection: Pfizer 2-dose = 85%, 1-dose = 55%; AZ 2-dose = 70%, 1-dose = 45%. |
The latest REACT-1 (UK) study [Imperial] saw an apparent drop in (aggregate) vaccine efficacy (VE) from 64% in round 12 (20 May to 7 June) down to 49% in the latest round 13 (24 June to 12 July) [via Deepti Gurdasani Twitter]. For two doses.
However, it should be noted that VE is a relative measure, contrasting incidence between those with and without vaccination, only. This will show a decline as a higher percentage of unvaccinated develop protection from past infection [Carl T. Bergstrom Twitter]. ~20% of the UK adult population has infection-specific antibodies. But this is quite likely to be significantly higher in the unvaccinated cohort, because: (i) they skew young, with a higher infection rate (maybe as high as 40%), (ii) less likely to bother getting unvaccinated if you know you'd already been infected (iii) correlation with less diligence about health (and protecting others).
This illusory effect may be bigger than the actual decline in protection from waning immunity, or vaccine immunity escape mutations in the Covid variant.
 |
| [Fig.3 - Gov.UK] Adults vaccinated as of 2021-08-08. |
(2) Reduction of transmission from breakthrough cases: is a vaccinated person who becomes infected (tests positive) as likely to spread that infection to others as an unvaccinated person?
In the most recent PHE report [GOV.UK], the viral loads (amount of virus DNA in swabs used for PCR testing) in vaccinated people with breakthrough infections was just as high as in the unvaccinated cases: 17.8 verses 18.0, respectively. The relevant graph (page 35, Fig.12) is very confusing to interpret, so I've not embedded it: higher "CT" value indicates lower viral load, with more RNA amplification cycles to reach detection. It's also comparing Alpha vs Delta variants, but using weird names for them.
In the most recent PHE report [GOV.UK], the viral loads (amount of virus DNA in swabs used for PCR testing) in vaccinated people with breakthrough infections was just as high as in the unvaccinated cases: 17.8 verses 18.0, respectively. The relevant graph (page 35, Fig.12) is very confusing to interpret, so I've not embedded it: higher "CT" value indicates lower viral load, with more RNA amplification cycles to reach detection. It's also comparing Alpha vs Delta variants, but using weird names for them.
Breakthrough infections may run a shorter duration of infectivity: PCR detectability down from 8.9 to 2.7 days duration [CDC presentation page 7, also see page 16 graph Medrxiv]. However, transmission is most likely early on, in a new case, before symptoms or self isolation [Deepti Gurdasani Twitter]. So, overall, we should probably treat breakthrough infections as about equally infectious.
(3) Number of previously infected - People developed Covid-19 antibodies from either infection or vaccination. Infections can be distinguished because the (Pfizer and AZ) vaccines only show the immune system spike proteins. Antibodies to these show up on a Roche S (for "Spike") finger prick serum test. Vaccines don't induce antibodies to the nucleocapsid protein, while those exposed to the virus itself will have them. This second protein structure is also on the virus's outer surface. But it's not as import an antigen to target, because the spike facilitates cell entry. So those testing positive with Roche N will have had infection only. While Roche S detects both infection and/or vaccination.
 |
| [Fig.4 - PHE week 31 report GOV.UK, via Twitter] Types of antibody (S or N, see above explanation) for different age groups in the UK, over time. We see the rising curves of spike protein anti-bodies in successive age groups, started from the oldest (lower graph). Also, higher levels of immunity from infection in younger age groups. Ultimately almost ~20% in 17-29 year olds, verses ~8% in over 70s. Showing more social contact in young adults and benefit of shielding of the elderly. |
The above agree quite closely with seroprevalence of blood donation samples, showing ~16.4% of these adults had been previously infected. From page 2 of PHE surveillance report week 31 [Gov.UK].
(4) How protective is past infection? - We could infer that past infections are very highly protective against subsequent infections, given that only ~1% of official cases are reinfections [Meaghan Kall Twitter]. This certainly does not mean 99% protection! For a start, we know that official case numbers for the the UK of ~4Mn greatly underestimate the number of actual infections. The anti-body prevalence of 17% (from above) implies at least ~11Mn previous infections. So reinfections could quite plausibly be 2.75 times higher, ~3% or more. Although, access to testing is not random; those who got tested before are more likely to go get tested again, verse those who didn't or couldn't before. So maybe the case undercounting isn't so significant.
Anyway, hypothetically, if past infection gave zero protection, we'd expect to see the same percent of reinfections as there are currently past infections. 4Mn is ~6% of our 66Mn UK population. So if we're only seeing 1% in practice, the odds are being reduced by around 6 fold. Which I think means ~83% effective...? This is extremely approximate for many reasons. However, a February 2021 study (so no Delta) of hospital staff in Oxford, UK, reportedly estimated ~89% protection from reinfection [NEJM].
Its been reported [Newsweek] that a (fairly small) CDC study showed previously infected people were more than twice as likely to get reinfected (in May-June 2021, so Alpha variant) if they didn't get a vaccine afterwards, too. However, previously infected people, topped up with just one vaccine dose showed a "hybrid" immunity stronger than non-infected people with 2 vaccine doses. A Rush University study showed 4 of 29 (~14%) of previously infected people had developed no detectable antibodies at all. Responding the same to vaccination as non-infected.
This all makes it very clear that past infection is far from 100% protective against transmission, as speculated in E.1 (above)!
(5) Waning immunity - Protective antibodies kick in about 3 weeks after a first dose of vaccine. They peak 2-3 weeks after the second dose. This small study saw (at 21-41 days) that Pfizer produced about 6 times higher concentration of antibodies than AstraZenica [UCL]. Also declining less, to about 1/2 at 70 days, verses 1/6 for AZ. Hence older people with AZ will be more in need of booster shots.
High levels of serum antibodies are 'neutralising' - they will immediately bind to and block all spread of viral particles between cells in your body. Avoiding symptoms or onwards transmission. Titers (concentration) of this (in blood) are highly predictive of protection against SARS-CVO-2 [Nature].
 |
| [Fig.5 - Nature, Fig. 1 a] Predictive modelling of the protection of vaccines, relative to "convalescent" (past infection) by looking at the level of neutralising antibodies they each produce in serum. This model slightly overestimates protectiveness of AZ's (ChAdOx1) from their part b graph. But otherwise close, with mRNA vaccines actually more protective (published May 2021, so data is pre-Delta, I think?). |
Antibodies always decline naturally, over time, as the pool of the particular immune B-Cells that are specialised to make their type, dwindle. These B-Cells retain a memory and continue to make anti-bodies at a low level for very many years. Ready to much more quickly ramp up production upon new exposure. Hence ongoing protection against severe illness. Also, B-Cells may travel to lymph nodes where they gain mutations that can enhance their ability to bind viral protein structures more tightly. This process is called "affinity maturation", and is apparently promoted by repeat exposure, as with booster injections [Nature].
So, it's not surprising to see vaccine's average level of protection against *infection* (and mild illness) fall over time, even without new variants.
The Israeli health ministry released data showing protection had dropped from 90%, at the start of their vaccination program in December 2020, to about 40% by late June. This was reported at beginning of July [Reuters]. as a drop from 93% to 64%, from reports in May vs June. By the end of July articles [CNBC] were declaring an even more concerning drop to just 39% effective (more than 1/2 as likely to be infected as the unvaccinated). Which might have implied drastically waning immunity (given Israel were fore-runners in vaccine role-out). And/or Delta escaping immunity more than expected.
However... As Dvir Aran (Israeli medical data professor) explains [Twitter]: It turns out that these drastic numbers were overwhelmingly down to a fluke of the new outbreak's location: in a predominantly elderly population, of an area that was 95% vaccinated. While they were wrongly using the national average rate, closer to ~60%. This really highlights the great difficulties of interpreting observational health data. Since mid-July, with the outbreak spreading more widely through Israel, they've been seeing an increasing separation between vax'd and unvax'd, which has so far raised calculated efficacy back up to 80% (against severe illness):
 |
| [Fig.6 - Dvir Aran Twitter] Flukey Israeli Covid incidence, now resolving. |
"Lies, damned lies, and statistics", heh. In trying to work out how much immunity wanes, there's also the confounding factor that virtually all countries vaccinated their elderly population first, so without adjusting for that one would obviously see lower immunity, longer from vaccination, as looking back in time also drastically increases average age. And early vaccinated young adults were often medical staff and workers more highly exposed to infection risk, confounding that [Nature].
Between countries, Israel also used the short (recommended), 3 week interval between doses, which is probably less effective than the UK's improvised 8 week schedule. One thing our authorities actually got right, despite much worry about deviation from the manufacturer's validation trials.
So how fast does effective immunity (against symptomatic infection) wane in practice? Including to previous infection...? 🤷♂ I don't know. Even if we assume exponential decay and there's a solid half-life for antibodies, of say, 2-3 months, the threshold for complete neutralisation is going to vary between people and their levels of exposure to the virus. Plus there's T-cell immunity, which is not so easily measured. And non-adaptive, i.e. innate, immunity that varies between people and ages.
(6) Rough calculation of current average UK immunity - Putting together our figures for the various aspects from above, including the more optimistic vaccine effectiveness figures from VEEP (Fig.2.b). With vaccine type and dose data taken from page 5 of MHRA's "summary of Yellow Card reporting" up to 28/07/2021 [GovUK, via Twitter]. I get a reasonable best case total population immunity figure of ~63%:
 |
| [Fig.7 - My Google Sheet] I've not considered boosted hybrid immunity, for those vaccinated *and* previously infected. But it's probably a fairly modest effect, in terms of epidemiology. And I'd guess it would be counterbalanced by waning immunity (which I've also not included). All other stats are the most optimistic I could find. Particularly childhood infections... There there's no major seroprevalence studies in <18 year old age groups. So infection rate in kids is a guestimation: I've used a the 60% "upper bound" number Meaghan Kall (PHE epidemiologist) suggested to me on [Twitter]. She was a co-author on a small study (2k samples) in March 2021, which found ~33% of urban secondary school pupils had N type antibodies [MedRxiv, via Shamez Ladhani Twiter]. So it's very likely we've passed 40%-50% since then, given the ongoing high infection rate in kids, for the last couple of months. Reasonable worst case population immunity figure I came up with was ~53%. And even if we were to finish up giving all adults, who've had 1st vaccine dose, their 2nd dose too, then (tragically) allow *all* kids to become infected (and assume that's 100% protective against reinfection), then we still only get to ~75%. Meaning that we really need to vax virtually all adults *and* probably have infections in many too (to boost that protection)... |
From my first graph (Fig.1) in section H of my previous blog post, we can see that we would need 80-90% population immunity to bring Detla's R0 to <1, reducing spread. That's without any NPIs (non pharmaceutical interventions, e.g. case isolation, distancing, masks, etc). Given the possible range of Delta's R0 of 5 to 9.5 (stated in CDC slide, below):
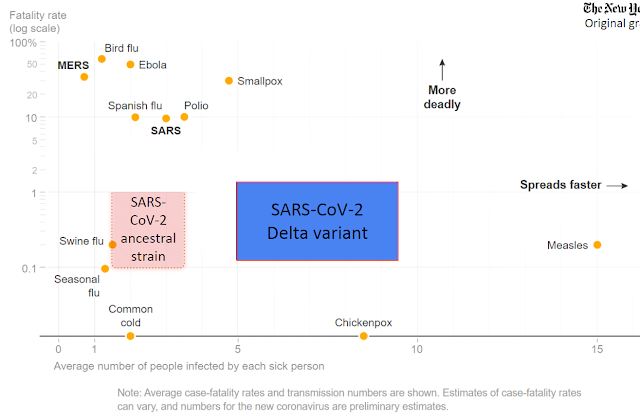 |
| [Fig.8 - CDC via NYTimes] Delta variant is way more contagious than all the flu types, common cold, polio, smallpox, etc. But its R0 number is very hard to pin down exactly, given that everywhere has varying NPIs and partial immunities differing across age groups and geographical areas. |
 |
| [Fig.9 - My illustration, adapted from a graph on CEMB] Taking our somewhat optimistic 63% population immunity figure, Delta's R0 of 5 to 9.5 translates to an effective R value of 1.8 to 3.5. Re must be 1 or below in order for cases to decline (without any NPIs). |
So, without current mitigations in place (masks, working from home, schools on holiday), we'd be back to the same kind of rate of case increase that we had with the original strain (R0 = 2.4 to 2.6), back before March 2020 lockdowns. If we were only facing the original strain, Re would be <1 and pandemic would be over (thus is the enormous importance of variants).
So it looks like our pandemic adapted behaviours are roughly halving Re. Keeping effective R close to 1, for now. But that's going to rise gradually as the population becomes less cautious. And suddenly tick up in with schools and football kicking off again, soon. Amping up our ongoing stealthy herd immunity by infection in kids and youngsters. 😨
◄B► "Herd Immunity Mythical" Headlines:
The same day I published my analysis (above), mainstream news [e.g. iNews, Guardian] also picked up on the fact that we can't hit population immunity to Delta (with current vaccines). Quotes from Professor Andrew Pollard were trumpeted, from his answer to MP's questions during an All Party Parliamentary Group (APPG) public zoom call [full video on Periscope]. Also used by controversial figures, like Robert W Malone [Twitter] and outright anti-vaxxers, pushing a narrative that vaccines have always been useless and herd immunity a lie, etc.
Pollard is the most heavyweight expert possible: an immunology professor at Oxford Uni, director of the Oxford Vaccine group [OVG] (that developed the 'AstraZeneca vaccine'), previous advisor to WHO, member of SAGE (since 2016) and chairs the JCVI (since 2013). But not the JCVI's Covid-19 committee, due to his involvement with vaccine development [Wikipedia].
 |
| [Fig.10 - Channel 4 News Twitter] |
Having watched through the whole APPG video conference (which was very informative, in various ways), these are my notes (off the top of my head, a few days later):
• Professor Andrew Pollard: was keen to pivot towards vaccinating the rest of the world. Which is absolutely correct, as a first order approximation to the truth. But equating that with not vaccinating any children in UK was suspect; playing the zero-sum game as a justification; that even a few million doses could immunise a small country somewhere. Hmm. {Update: From his [Guardian] article, I think he's trying to head off the UK stockpiling most of the extra doses it's ordered, for mass booster shots.}
• Professor Paul Hunter: is also very experienced and had some interesting perspective on Corona Viruses becoming endemic. Essentially common colds reinfecting each person (in the UK) about every 4 years, as they slowly mutate. Equating this to our situation with SARS-COV-2, but glossing over the part where this is still an very damaging illness, with no sign of variants moving in the direction of innocuous common colds, yet.
I think he said the same as Pollard, with regards to UK having no control over new variants. Which is largely true, that we have a small population, compared to the number of bodies, globally, incubating Covid (e.g. India alone where about 15 times our population already had Delta). But talk of his "grandchildren's grandchildren" still getting Covid is total hyperbole! Totally ignoring UK's early 2020 resignation to mass infection (with targeted protection), being shown to be ludicrously unimaginative, when we started rolling out vaccination under 9 months later. There's no way we don't get more game changing vaccine/bio-tech in the next year or so. So short sighted of them.
Hunter also implied, in passing, that Long Covid is either organ damage or psychological! So it sounds like both of these men (and a majority on JCVI) are aligned with the BPS school of (wrong) thought on the cause of ME/CFS and 'Post Viral Fatigue', etc.
• Professor Devi Sridhar: seems to have the most incisively balanced perspective. Having been zero Covid in since ~April 2020, she's now trying coax the public into cautious resumption of activity [Guardian, via Twitter]. In the Zoom call, she was essentially pointing out the false dichotomy between vaccinating young and boosters for UK's vulnerable, verses sending doses abroad to the majority of the world with little/no vaccination so far. The solutions to that are different (waivers and outward investment, COVAX, etc), with only a relatively small number of extra doses now needed here. mostly Pfzier (or Moderna) which need a cold chain, so developing countries often can't make use of them anyway.
• Dr Ayoade Alakija: really pleased me, in calling out the jaw dropping hubris of the guys who'd both said there's nothing the UK can do about the advent of new variants, given that we birthed the Alpha (AKA "Kent") variant, here! The globally dominant variant until Delta. She made a whole lot of sense overall, and offered an external perspective on the UK from Africa.
• Dr Gregg Gonsalves: from New York, did great in really banging the drum, pushing for to waive patents and build up mRNA vaccine production capacity around the world (WHO's initiative, I think).
• Dr Ruchi Sinha: was irrelevant for most questions, but pointed out that NHS paediatric ICU (part of her remit as consultant paediatric intensivist) provision is being increasingly stretched.
 |
| [Fig.11 - John Barrett Twitter] It's been pointed out that those advocating for Covid elimination have been vindicated, in a way. The Alpha variant is effectively gone from the UK, now. The immediate retort is that it was pushed out by Delta (as Deepto Gurdasani replied [Twitter], confusingly). But that's only indirectly, marginally true... We already had Alpha under control with the Christmas lockdowns, declining steadily even as the vaccination program really got under way. Now we have even higher population immunity to Alpha (because our vaccines are a lot more effective against it) and its R0 value is distinctly lower than Delta (both somewhere in the 70s). So, in conjunction with our remaining NPIs, that is what has really killed Alpha off. Only a very small percent of the population had actually contracted (and developed immunity from) Delta, by June, when Alpha died. Very minimal direct interaction. One can easily approximate them as separate epidemics anyway. At most, the delay in easing Stage 4 restrictions (due to Delta's rise) helped slightly. Like Covid measures, in general, squashed flu cases and RSV, last winter. |
◄C► Vaccine Effectiveness (VE) Updates (2021-08-19):
Early Israeli data reportedly shows "a 4.6-fold risk reduction in infection 10+ days after 3rd dose" [Dvir Aran Twitter]. So the US announcement [e.g. Reuters] of booster shots for all (who will accept them), 8 months on from 2nd doses, is probably justified by science (at least in the most elderly). These are to be only mRNA (Pfizer, Moderna), but it may still further set back efforts to give developing countries any vaccine protection at all! (I think most will therefore just 'take it on the chin', as India was quietly ravaged by Delta.)
 |
| [Fig.12.a - FT via Eric Topol Twitter] Apparently, further study results (and summaries) of VE are in line with 50-60% protection of 2-doses against infection/symptoms. Significantly lower than the best case figures I used in my calculation above (so presumably bringing population immunity down). More figures in this table [Fig.12.b - Eric Topol Twitter]: |
 |
| [Fig.13 - Natalie E Dean Twitter] How vaccine efficacy is calculated. |
 |
| [Fig.14 - Covid Data Science, via Carl T Bergstrom Twitter] Demonstrating the how naïve VE calculations create strange artefacts due to greatly differing rates of incidence and vaccination status across the ages. Stratifying the Israeli vaccine efficacy (against severe disease) data, into just two age ranges, has the unintuitive effect of increasing the final figure from 68% (whole population) to 92% (under 50s) and 85% (over 50s). So UK estimates may be too pessimistic for this reason, too. Good news - maybe my optimistic calculation is not so far out. |
◄D►Next - Delta's rise, global vaccination and IP waiver, battle over Kids, Long Covid...


No comments:
Post a Comment
I'm very happy to see comments, but I need to filter out spam. :-)